Functional Genomics
This is the page description.
Elucidating How Genotype leads to Phenotype in Cardiometabolic and kidney Disease
Unbiased human-based discovery efforts, such as genome-wide and exome-wide association studies, have identified many genetic loci for complex, disease-relevant traits. These genetics studies have provided invaluable data implicating novel loci in disease development and progression, but require functional follow-up to elucidate the mechanistic underpinnings driving the associated findings. A focus of the lab is to interrogate, through experimental wet-bench approaches, the functional significance of novel loci for cardiometabolic traits in the hopes of gaining new insights into pathways relevant to disease.
In particular, we are studying the role of two genomic loci, A1CF and APOL1, at the intersection of kidney and cardiovascular disease.
A1CF is a gene encoding the RNA-binding protein APOBEC1 complementation factor and recently implicated as a locus for (1) elevated plasma triglycerides (Liu et al., Nature Genetics 2017), (2) estimated glomerular filtration fraction in non-diabetic individuals (Pattaro et al., Nature Communications 2016), and (3) serum urate (Kottgen et al., Nature Genetics 2013). We have already discovered that A1CF's actions extend beyond its canonical role of facilitating the editing of APOB mRNA, and we are currently integrating studies using animal and human cellular models to investigate how A1CF contributes to these associated traits.
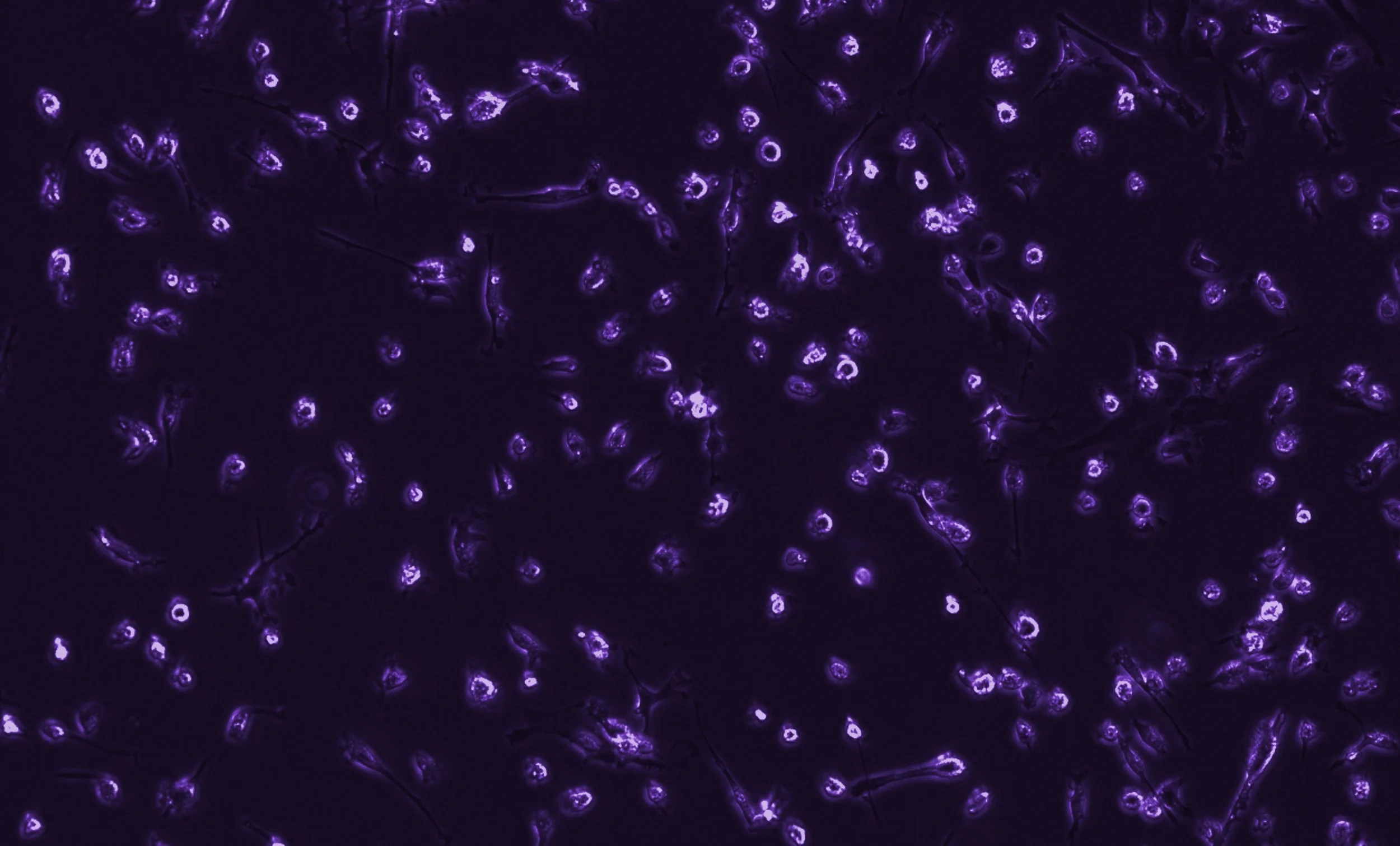
APOL1 is a gene encoding the trypanolytic factor Apolipoprotein-L1. Although the kidney disease risk variants (termed G1 and G2) confer a heterozygous survival advantage for African sleeping sickness, homozygosity or compound heterozygosity for these coding variants are associated with increased risk of chronic kidney disease. Whether the high-risk genotype also associates with increased risk of cardiovascular disease remains unclear due to conflicting observational studies. Because APOL1 is primate-specific in expression, our main focus is on human iPSC-based modeling of the variants, leveraging CRISPR-Cas9 genome editing technology to study the variants in their native genomic locus. The first publication from our lab demonstrates how an iPSC-derived kidney organoid model system, combined with single-cell transcriptomics, can reveal cell-specific insights into how the G1/G1 genotype alters the stress response. APOL1 is also expressed in multiple cell types and tissues, leading us to recognize that disease caused by the risk variants may not be limited to podocyte and tubular cells (kidney cells) in origin. Since the risk variants evolved in the context of innate immunity, we are investigating how the high-risk APOL1 genotype alters the phenotype and function of macrophages, which are significant contributors to kidney and cardiovascular disease.